A website called The Markup – funded by the same foundation that is providing financial support to organizations that are looking to add for-profit corporations to the donation and transplant policy making process and are interested in competing for contracts to run the national system – recently published a story about a lawsuit filed almost five years ago by a small number of transplant centers.
The transplant centers are seeking to reverse the successful liver patient-centric allocation reforms despite the fact the reforms have led to a sharp increase in the number of lifesaving liver transplants, especially among the most medically urgent patients. The lawsuit alleges that the reforms would have negative financial consequences to their transplant centers.
In The Markup story, the reporter repeats the plaintiff’s attorneys arguments wholesale and alleges that a “secretive scheme” was concocted by the federal government, the national Organ Procurement and Transplant Network and Organ Procurement Organizations to unfairly change the allocation system to prioritize the needs of the sickest liver patients at the expense of the transplant center’s finances. Of course, no secret scheme existed and the public process of adopting the new allocation system while contentious at times, passed by a vote of the OPTN board by a wide margin, 30 votes (including all of the patient representatives on the Board at that time) to 7 votes.
NEDS President and CEO Alex Glazier was a longtime supporter of allocation reform that would be more equitable and patient-centric, prioritizing the needs of the sickest patients first rather than the geographic location of where patients lived.
When contacted by The Markup about her role in the allocation reform process, Alex Glazier emailed the reporter a substantive overview and a lengthy quote regarding the liver allocation reform process. Much of what was provided to the reporter was ignored, so in the interest of transparency and accuracy, NEDS provides the full text of the email sent to the reporter below.
NEDS has requested that the reporter include the full “on the record” statement provided rather than the one part of one sentence she picked to published but she responded that “the article includes the relevant portions.” You can evaluate her statement for yourself.
—————————————————————
Hi Malena –
Thanks for reaching out.
In response, the quoted and italicized portion is on the record and below that is some additional information and context for background. Please let me know if you have any questions.
“Providing an opinion and input on policy is the fiduciary responsibility and expected of OPTN board members which I was a nationally elected member of in 2016-2018. Plaintiffs in this lawsuit targeted only a few individuals in their discovery process then cherry-picked documents to make it look like only a small number were part of the policy discussions when, in fact in this case, many dozens including transplant professionals from the plaintiff hospitals were involved in the same discussions and provided their perspective to the OPTN Board, UNOS and HRSA. It is inexplicable that these transplant hospitals persist with this lawsuit, especially when the sickest transplant patients in our nation are being helped by this more equitable, patient-centric allocation policy reform endorsed by the National Academy of Science.”
————
[FOR BACKGROUND AND CONTEXT]
During the allocation reform work that took place in 2017-2018, I was a nationally elected member of the OPTN Board and took my responsibilities seriously to advocate for policies that met legal and regulatory obligations under NOTA and the Final Rule and that I felt most equitably served the interest of all patients everywhere. As a fiduciary of the Board of the OPTN at the time, it was my responsibility to provide my opinion and I gave my opinion on why a patient-centric allocation policy was more equitable and legally complaint than DSA-based policies to other Board members, to stakeholders and to individuals at UNOS and HRSA all of whom were free to accept or disregard my position.
The materials plaintiffs have amassed in this lawsuit are the result of their target on me and select others who advocated for reform. They did not request discovery over emails from all the OPTN Board members at the time, or even emails of all the OPTN Executive Committee members. Only mine. They did not depose any other OPTN Board member. Only me. As a result, the materials unsealed by plaintiffs are not even close to the full body of discussions that occurred between OPTN Board members and other stakeholders related to allocation reforms of lung or liver policy and instead these documents were cherry picked to give the appearance that only a few individuals were involved in order to construct a false narrative. What they fail to show are the many communications other members of the OPTN Board had, advocating their own positions to other board members, stakeholders and to individuals at UNOS and to HRSA. The plaintiffs then attempt to describe my communications as unusual or different from conversations they themselves and many others were having. This is particularly disingenuous given that the plaintiffs have not yet had to produce any discovery nor have they pursued discovery over communications other than mine.
The plaintiffs were outvoted by a huge majority of the OPTN Board (30-7) in passing the liver policy equity reform including every patient representative on Board at the time, and instead of accepting that result the plaintiffs are desperately trying to claim without any evidence that the vote was somehow rigged at the direction of a couple individuals when the truth is the entire transplant community, policy experts, the OPTN Board and HRSA were actually involved in this debate for decades. Copied below is the context and history of this allocation reform I previously provided to you and your editor last March.
It is inexplicable that 14 centers continue to waste time and resources on this lawsuit years later despite the fact that patients are being helped by this more equitable policy including an increase in access to liver transplants at many of the plaintiff transplant programs (see for example, VA Commonwealth which has had a 100% increase in deceased liver donor transplants since the liver equity reform policy was implemented). What remedy do these plaintiffs seek?
I had no inside knowledge nor did I have anything to do with the NY, MA, CA lawsuits –any suggestion in your story to the contrary would be entirely and knowingly inaccurate and false. I have never advocated for the use of lawsuits to change allocation policy and I have never been a member of or affiliated with the Greater NY Hospital Association or had any involvement in the cases or contact with counsel for the plaintiffs in either the NY lung or NY/MA/CA liver lawsuits. It was obvious and foreseeable as a health law attorney that these lawsuits would be filed because there were strong legal arguments that the DSA-based policies were noncompliant and patients waiting in those areas were being harmed as a result.
————
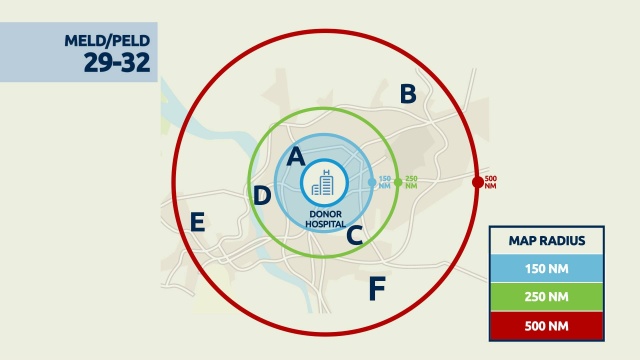
The GAO issued a lengthy report on the history of the development of the lung and liver distribution polices; it is a straightforward, factual reporting of the facts of the policy development. As the GAO described it, “liver allocation policy changed from a system that, in general, offered deceased donor livers first to the candidates with the highest level of illness within the deceased donor’s DSA and OPTN region before offering them outside the region, to a system that allocates livers based on a candidate’s level of illness and distance from the donor hospital.” Further, the GAO noted when each policy change was proposed, with specific dates:
“The impetus for the changes resulting in [lung and liver] allocation policy varied. Specifically, the impetus for the changes resulting in the current liver allocation policy was an HHS directive following the agency’s receipt of a critical comment regarding the use of DSAs and OPTN Regions in the 2013-2020 liver allocation policy and the 2017 liver allocation policy. The impetus for the changes resulting in the current lung allocation policy was two-fold. First, a federal district court ordered HHS to initiate an emergency review of the lung allocation policy. Second, HRSA directed OPTN to initiate an emergency review of the lung allocation policy in accordance with the court order and as a first step in responding to a critical comment asking HHS to require OPTN to set aside portions of the lung allocation policy that utilize DSAs. The impetus for the changes that resulted in the 2017 liver allocation policy was a November 2012 OPTN Board directive to address geographic disparities.”
This overview from GAO directly undercuts any claim that the change in policies were somehow at the direction of a few individuals; removing DSA from allocation policies and broader sharing of organs has been publicly discussed, endorsed and recommended by multiple bodies for decades:
- 1999 Institute of Medicine issues a report recommending the broader sharing of livers
- 2000 Federal regulation – the OPTN Final Rule – requires that organ allocation policies “shall not be based on the candidate’s place of residence or place of listing”
- 2002 MELD/PELD measure of patient illness acuity voted by the OPTN Board into liver allocation policy
- 2010 HHS Secretary’s Advisory Committee on Organ Transplantation (ACOT) directive “to eliminate geographic inequity” and “to ensure the OPTN develops evidence-based allocation policies which are not determined by arbitrary administrative boundaries such as OPO
- 2012 OPTN Board directive to address geographic disparities
- 2017 Federal district court order directs HHS to initiate emergency review of lung allocation policy based on the use of DSA.
- 2017 Distance from donor hospital is geographic boundary implemented for allocation of lungs
- 2018 HHS directs OPTN to develop policies for all organ types that remove DSA-based allocation and are consistent with the OPTN Final Rule.
- 2018 OPTN Board approves geographic principles of allocation to incorporate distance into allocation policies for all organ types in a consistent and legally compliant manner
- 2018 Distance from donor hospital is geographic boundary approved by OPTN Board for allocation of livers
- 2019 Distance from donor hospital is geographic boundary approved by OPTN Board for allocation of hearts
- 2019 Distance from donor hospital is geographic boundary approved by OPTN Board for allocation of kidneys
- 2022 National Academy of Sciences endorses OPTN broader sharing reforms to reduce geographic inequities and recommends accelerated implementation of continuous distribution frameworks.
Alexandra K. Glazier, JD MPH (she/her)
President & CEO
New England Donor Services